Brain surgery simulator
Japanese/English
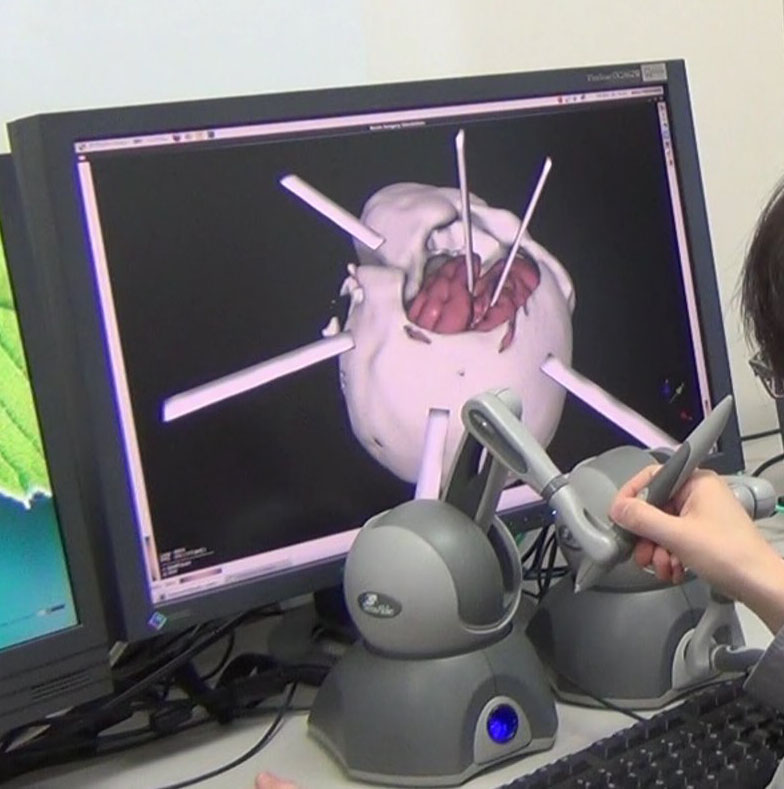
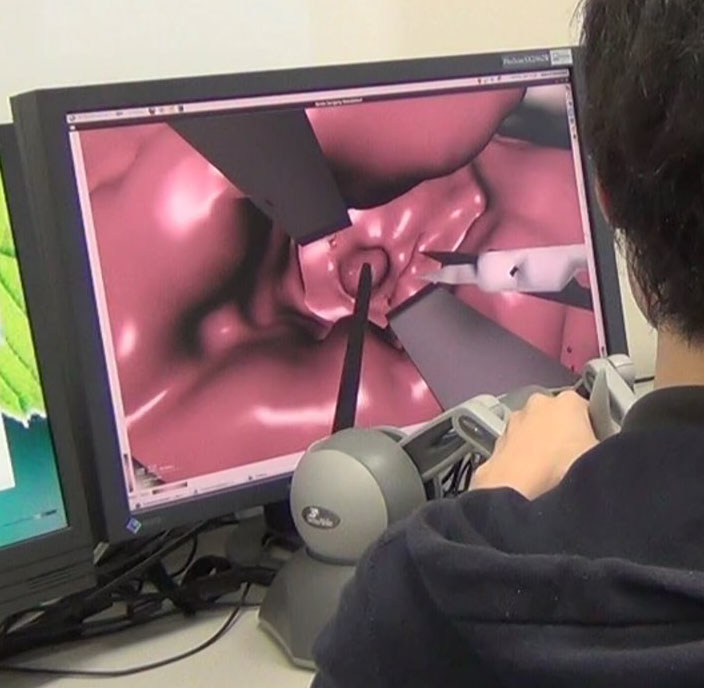
Fig. 1 Brain surgery simulator under development.
In recent years, surgical simulators are attracting rising attention as an efficient method to train surgeons.
A haptic surgical simulator provides an immersive surgical environment by performing real-time simulation of organ behavior and displaying contact force between surgery instruments and organs via a haptic device.
The following applications are expected to surgical simulators.
1. Surgery training
Experienced doctors make unerring judgments in surgery obtaining crucial information such as lesion state and nerves location not only from view but also from haptic information.
Therefore, haptic perception should be well trained in surgery simulation.
Traditional training using animals or organ models made of silicon or rubber is not sufficient to train such haptic perception, because characteristics of animal tissue and silicon rubber rapidly vary with the passage of time.
Furthermore, it is impossible to correctly reproduce the individual case of patients using such models or animals.
As a new method, a surgical simulator is expected to construct various surgical situations, and to perform an efficient training by warning wrong treatment or giving advice based on situations.
In addition, it is possible to iteratively practice a particular surgery because the characteristics of the computer model do not change as time passes.
2. Preoperative planning and verification of the plan
It is necessary to take appropriate operation in accordance with the individual cases of a patient. Therefore, CT or MRI scan is generally performed before a surgery in order to visualize the lesions and organs.
3D visualization from tomographic image is useful for preoperative surgery planning. Therefore, surgical simulators can construct a virtual surgical environment using patient-specific model which is reconstructed from tomographic data. As a result, surgeons can review incision in the skin and bone or approaches of organ retraction by simulation, and practice operations with patient-specific model.
We are researching and developing a brain surgery simulator.
Cerebrovascular disease is a major cause of death and brain surgeries may have great effects on the life of patients.
Therefore, the introduction of a brain surgical simulator is expected to increase safety in a brain surgery.
Study results
1. Deformation and fracture model for the blunt dissection operation simulation [6], [7]
Dissection is one of the basic operations in surgeries.
There are two types of dissection: a sharp dissection (cutting) using scissors and blunt dissection which destroys selectively using concentrate stress on the fragile part of organs.
Blunt dissection is required experience to force adjustment, because there is a risk of causing damage to the critical parts by incorrect operation.
In our laboratory, we have developed a deformation and fracture model for performing a blunt dissection in the surgical simulator.
This model is based on the stress analysis by the finite element method, and it is suitable for representation of blunt dissection.
Furthermore, we have realized a stable fracture simulation by avoiding instability associated with the progress of fracture.
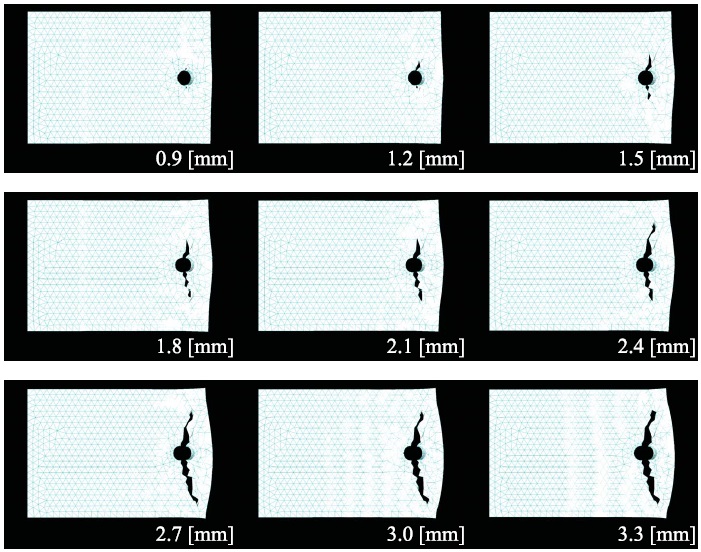
Fig. 2 The fracture simulation caused by developed fracture model [7].
2. Viscoelastic model development and body tissue parameters identification [5], [8]
For performing deformation calculation in consideration of the viscoelasticity of the brain parenchyma, we have developed a viscoelastic model and identified viscoelastic parameters.
Viscoelastic model is based on finite element method and can be combined with fracture model developed by our laboratory.
Additionally, we did mechanical characterization tests of biological tissues, and we conducted a numerical model evaluation and proposal of the viscoelastic parameters identification method based on the test data.
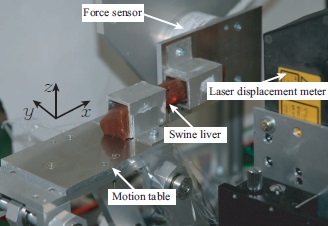
Fig. 3 Mechanical characterization testing of biological tissue [5].
Current study
Two surgery scenes are reproduced by the simulation:
- opening a brain fissure,
- extirpation of a tumor on insula.
Two-handed operation is possible in the above simulation. The current research themes are:
- a parallel computing technology to realize the real-time simulation of large-scale brain model,
- an accurate model than ever including viscoelasticity and destruction.
Reference
- Takuya Kameyama, Teppei Tsujita, Atsushi Konno, Xin Jiang, Satoko Abiko, and Masaru Uchiyama, Displaying Cutting Force of Soft Tissue Using MR Fluid for Surgical Simulators, Proceedings of the IEEE Haptics Symposium, Houston, Texas, pp. 283-288, USA, February 23-26, 2014.
- Atsushi Konno, Masano Nakayama, Xiaoshuai Chen, Akira Fukuhara, Kazuya Sase, Teppei Tsujita, and Satoko Abiko, Development of a Brain Surgery Simulator, The International Symposium on Interdisciplinary Research and Education on Medical Device Developments, pp. 29-32, Hirosaki, Japan, September 12-13, 2013.
- Teppei Tsujita, Kazuya Sase, Atsushi Konno, Masano Nakayama, Chen Xiao Shuai, Koyu Abe, Masaru Uchiyama, Design and Evaluation of an Encountered-type Haptic Interface Using MR fluid for Surgical Simulators, Advanced Robotics, Vol. 27, No. 7, pp. 525-540, DOI:10.1080/01691864.2013.777013, 2013.
- Teppei Tsujita, Manabu Ohara, Kazuya Sase, Atsushi Konno, Masano Nakayama, Koyu Abe and Masaru Uchiyama, Development of a Haptic Interface Using MR Fluid for Displaying Cutting Forces of Soft Tissues, Proceedings of 2012 IEEE International Conference on Robotics and Automation, RiverCentre, Saint Paul, Minnesota, USA, pp. 1044-1049, May 14-18, 2012.
- Xiaoshuai Chen, Masano Nakayama,Teppei Tsujita, Xin Jiang, Satoko Abiko, Koyu Abe, Atsushi Konno and Masaru Uchiyama, Identification of Physical Properties of Swine Liver for Surgical Simulation Using a Dynamic Deformation Model, Proceedings of 2011 IEEE/SICE International Symposium on System Integration, C9-2, pp.655-660, Kyoto, Japan, December 20-22, 2011.
- Masano Nakayama, Satoko Abiko, Xin Jiang, Atsushi Konno and Masaru Uchiyama, Stable Soft Tissues Fracture Simulation for Surgery Simulator, Journal of Robotics and Mechatronics, Vol. 23, No. 4, pp. 589-597, August 2011.
- Masano Nakayama, Atsushi Konno, Xin Jiang, Satoko Abiko, and Masaru Uchiyama, Linear Elastic Fracture Model for Brain Surgery Simulation, Proceedings of 2011 IEEE/ASME International Conference on Advanced Intelligent Mechatronics, Budapest, Hungary, pp. 333-338, July 3-7, 2011.
- Xiaoshuai Chen, Masano Nakayama, Atsushi Konno, Xin Jiang, Satoko Abiko, and Masaru Uchiyama, Simulation of Surgical Dissection Using a Dynamic Deformation Model, Proceedings of 2010 IEEE/SICE International Symposium on System Integration, Sendai, Japan, pp. 90-95, December 21-22, 2010.
- Shohei Fujino, Daisuke, Sato, Koyu Abe, Atsushi Konno, and Masaru Uchiyama, Displaying Feeling of Cutting by a Micro-Scissors Type Haptic Device, Proceedings of 2008 IEEE International Conference on Robotics and Automation, Pasadena, USA, pp. 2067-2072, May 19-23, 2008.
[Home] [Publications]
Last update: 2014/04/22